Juvenile Nasopharyngeal Angiofibroma: Difference between revisions
Jack.Dewey (talk | contribs) |
Jack.Dewey (talk | contribs) mNo edit summary |
||
| Line 31: | Line 31: | ||
=== Disease Etiology === | === Disease Etiology === | ||
===Epidemiology=== | ===Epidemiology=== | ||
Juvenile nasopharyngeal angiofibroma has been reported to be the most common benign neoplasm of the nasopharynx in young males. It accounts for 0.05% to 0.5% of all head and neck tumors, with a reported incidence of 1 in 5,000 to 1 in 60,000 in the US annually.<ref name="Boghani 2013">Boghani Z, Husain Q, Kanumuri VV, Khan MN, Sangvhi S, Liu JK, Eloy JA. Juvenile nasopharyngeal angiofibroma: a systematic review and comparison of endoscopic, endoscopic‐assisted, and open resection in 1047 cases. The Laryngoscope. 2013 Apr;123(4):859-69.</ref><ref name="Ferouz 1995">Ferouz AS, Mohr RM, Paul P. Juvenile nasopharyngeal angiofibroma and familial adenomatous polyposis: an association?. Otolaryngology—Head and Neck Surgery. 1995 Oct;113(4):435-9.</ref><ref name="Huang 2014">Huang Y, Liu Z, Wang J, Sun X, Yang L, Wang D. Surgical management of juvenile nasopharyngeal angiofibroma: analysis of 162 cases from 1995 to 2012. The Laryngoscope. 2014 Aug;124(8):1942-6.</ref> It classically presents in adolescent males, with an typical age of presentation between 13 and 22 years old.<ref name ="Newman 2023">Newman M, Nguyen TB, McHugh T, Reddy K, Sommer DD. Early-onset juvenile nasopharyngeal angiofibroma (JNA): a systematic review. Journal of Otolaryngology-Head & Neck Surgery. 2023 Dec;52(1):s40463-023.</ref> | Juvenile nasopharyngeal angiofibroma has been reported to be the most common benign neoplasm of the nasopharynx in young males. It accounts for 0.05% to 0.5% of all head and neck tumors, with a reported incidence of 1 in 5,000 to 1 in 60,000 in the US annually.<ref name="Boghani 2013">Boghani Z, Husain Q, Kanumuri VV, Khan MN, Sangvhi S, Liu JK, Eloy JA. Juvenile nasopharyngeal angiofibroma: a systematic review and comparison of endoscopic, endoscopic‐assisted, and open resection in 1047 cases. The Laryngoscope. 2013 Apr;123(4):859-69. https://doi.org/10.1002/lary.23843</ref><ref name="Ferouz 1995">Ferouz AS, Mohr RM, Paul P. Juvenile nasopharyngeal angiofibroma and familial adenomatous polyposis: an association?. Otolaryngology—Head and Neck Surgery. 1995 Oct;113(4):435-9. https://doi.org/10.1016/S0194-59989570081-1</ref><ref name="Huang 2014">Huang Y, Liu Z, Wang J, Sun X, Yang L, Wang D. Surgical management of juvenile nasopharyngeal angiofibroma: analysis of 162 cases from 1995 to 2012. The Laryngoscope. 2014 Aug;124(8):1942-6. https://doi.org/10.1002/lary.24522</ref> It classically presents in adolescent males, with an typical age of presentation between 13 and 22 years old.<ref name ="Newman 2023">Newman M, Nguyen TB, McHugh T, Reddy K, Sommer DD. Early-onset juvenile nasopharyngeal angiofibroma (JNA): a systematic review. Journal of Otolaryngology-Head & Neck Surgery. 2023 Dec;52(1):s40463-023. https://doi.org/10.1186/s40463-023-00687-w</ref> | ||
=== Genetics === | === Genetics === | ||
There is no identified definitive genetic locus that predisposes patients to JNA's. However, there have been a number of studies looking at the various genetic components that could influence their formation.<ref name="Doody 2019">Doody J, Adil EA, Trenor III CC, Cunningham MJ. The genetic and molecular determinants of juvenile nasopharyngeal angiofibroma: a systematic review. Annals of Otology, Rhinology & Laryngology. 2019 Nov;128(11):1061-72.</ref> Due to fact that JNA's classically form in adolescent males, there have been several studies focused on the possible hormonal influence on their formation and growth. JNA's tend to have an abundance of progesterone and estradiol, but a relatively lower concentration of testosterone and dihydrotestosterone.<ref name="Kumagami 05 1993">Kumagami H. Estradiol, dihydrotestosterone, and testosterone in juvenile nasopharyngeal angiofibroma tissue. American Journal of Rhinology. 1993 May;7(3):101-4.</ref><ref name="Kumagami 01 1993">Kumagami H. Sex hormones in juvenile nasopharyngeal angiofibroma tissue. Auris Nasus Larynx. 1993 Jan 1;20(2):131-5.</ref> Supplemental testosterone was trialed in JNA patients, but both tumor growth<ref name="Johnsen 1966">Johnsen S, Kloster JH, Schiff M. The action of hormones on juvenile nasopharyngeal angiofibroma. Acta Oto-Laryngologica. 1966 Jan 1;61(1-6):153-60.</ref> and tumor recurrence<ref name="Riggs 2010">Riggs S, Orlandi RR. Juvenile nasopharyngeal angiofibroma recurrence associated with exogenous testosterone therapy. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck. 2010 Jun;32(6):812-5.</ref> have been documented. | There is no identified definitive genetic locus that predisposes patients to JNA's. However, there have been a number of studies looking at the various genetic components that could influence their formation.<ref name="Doody 2019">Doody J, Adil EA, Trenor III CC, Cunningham MJ. The genetic and molecular determinants of juvenile nasopharyngeal angiofibroma: a systematic review. Annals of Otology, Rhinology & Laryngology. 2019 Nov;128(11):1061-72. https://doi.org/10.1177/0003489419850194</ref> Due to fact that JNA's classically form in adolescent males, there have been several studies focused on the possible hormonal influence on their formation and growth. JNA's tend to have an abundance of progesterone and estradiol, but a relatively lower concentration of testosterone and dihydrotestosterone.<ref name="Kumagami 05 1993">Kumagami H. Estradiol, dihydrotestosterone, and testosterone in juvenile nasopharyngeal angiofibroma tissue. American Journal of Rhinology. 1993 May;7(3):101-4. https://doi.org/10.2500/105065893781976393</ref><ref name="Kumagami 01 1993">Kumagami H. Sex hormones in juvenile nasopharyngeal angiofibroma tissue. Auris Nasus Larynx. 1993 Jan 1;20(2):131-5. https://doi.org/10.1016/S0385-8146(12)80240-9</ref> Supplemental testosterone was trialed in JNA patients, but both tumor growth<ref name="Johnsen 1966">Johnsen S, Kloster JH, Schiff M. The action of hormones on juvenile nasopharyngeal angiofibroma. Acta Oto-Laryngologica. 1966 Jan 1;61(1-6):153-60. https://doi.org/10.3109/00016486609127052</ref> and tumor recurrence<ref name="Riggs 2010">Riggs S, Orlandi RR. Juvenile nasopharyngeal angiofibroma recurrence associated with exogenous testosterone therapy. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck. 2010 Jun;32(6):812-5. https://doi.org/10.1002/hed.21152</ref> have been documented. | ||
=== Histology === | === Histology === | ||
| Line 78: | Line 78: | ||
! Classification System !! style=width:15em | Stage I !! style=width:15em | Stage II !! style=width:15em | Stage III !! style=width:15em | Stage IV !! style=width:15em | Stage V | ! Classification System !! style=width:15em | Stage I !! style=width:15em | Stage II !! style=width:15em | Stage III !! style=width:15em | Stage IV !! style=width:15em | Stage V | ||
|- | |- | ||
| Andrews (1989)<ref name="Andrews 1989">Andrews JC, Fisch U, Aeppli U, Valavanis A, Makek MS. The surgical management of extensive nasopharyngeal angiofibromas with the infratemporal fossa approach. The Laryngoscope. 1989 Apr;99(4):429-37.</ref> || Confined to NP || Invading one of the following with evidence of bony erosion: PPF, MS, ES, or SS || Invading ITF or orbit<br><br>'''IIIa''': No intracranial extension<br>'''IIIb''': Extradural (parasellar) extension || Intradural extension<br><br>'''IVa''': No infiltration of CS, PF, or OC<br>'''IVb''': Infiltration of CS, PF, or OC || -- | | Andrews (1989)<ref name="Andrews 1989">Andrews JC, Fisch U, Aeppli U, Valavanis A, Makek MS. The surgical management of extensive nasopharyngeal angiofibromas with the infratemporal fossa approach. The Laryngoscope. 1989 Apr;99(4):429-37. https://doi.org/10.1288/00005537-198904000-00013</ref> || Confined to NP || Invading one of the following with evidence of bony erosion: PPF, MS, ES, or SS || Invading ITF or orbit<br><br>'''IIIa''': No intracranial extension<br>'''IIIb''': Extradural (parasellar) extension || Intradural extension<br><br>'''IVa''': No infiltration of CS, PF, or OC<br>'''IVb''': Infiltration of CS, PF, or OC || -- | ||
|- | |- | ||
| Chandler (1984)<ref name="Chandler 1984">Chandler JR, Moskowitz L, Goulding R, Quencer RM. Nasopharyngeal angiofibromas: staging and management. Annals of Otology, Rhinology & Laryngology. 1984 Jul;93(4):322-9.</ref> || Confined to NP || Extension into the nasal cavity, SS, or both || Extension into any of the following: antrum, ES, PMF, ITF, orbit, or cheek || Intracranial extension || -- | | Chandler (1984)<ref name="Chandler 1984">Chandler JR, Moskowitz L, Goulding R, Quencer RM. Nasopharyngeal angiofibromas: staging and management. Annals of Otology, Rhinology & Laryngology. 1984 Jul;93(4):322-9. https://doi.org/10.1177/000348948409300408</ref> || Confined to NP || Extension into the nasal cavity, SS, or both || Extension into any of the following: antrum, ES, PMF, ITF, orbit, or cheek || Intracranial extension || -- | ||
|- | |- | ||
| Onerci (2006)<ref name="Onerci 2006">Onerci M, Oğretmenoğlu O, Yücel T. Juvenile nasopharyngeal angiofibroma: a revised staging system. Rhinology. 2006 Mar 1;44(1):39-45.</ref>|| Nose, NP, ES, and SS or minimal extension into PMF || MS involvement, full occupation of PMF, extension to anterior cranial fossa, limited extension into ITF || Deep extension into cancellous bone at pterygoid base or body and GW of sphenoid, significant lateral extension into ITF or pterygoid plates, orbital involvement, CS obliteration || Intracranial extension between pituitary gland and ICA, tumor localization lateral to ICA, middle fossa extension and extensive intracranial extension || -- | | Onerci (2006)<ref name="Onerci 2006">Onerci M, Oğretmenoğlu O, Yücel T. Juvenile nasopharyngeal angiofibroma: a revised staging system. Rhinology. 2006 Mar 1;44(1):39-45. PMID: 16550949</ref>|| Nose, NP, ES, and SS or minimal extension into PMF || MS involvement, full occupation of PMF, extension to anterior cranial fossa, limited extension into ITF || Deep extension into cancellous bone at pterygoid base or body and GW of sphenoid, significant lateral extension into ITF or pterygoid plates, orbital involvement, CS obliteration || Intracranial extension between pituitary gland and ICA, tumor localization lateral to ICA, middle fossa extension and extensive intracranial extension || -- | ||
|- | |- | ||
| Radkowski (1996)<ref name="Radkowski 1996">Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma: changes in staging and treatment. Archives of Otolaryngology–Head & Neck Surgery. 1996 Feb 1;122(2):122-9.</ref>|| '''IA''': Confined to nose or NP<br>'''IB''': Extends into one or more sinuses || '''IIa''': Minimal extension into medial PMF<br>'''IIb''': Full occupation of PMF with local mass effect<br>'''IIc''': Extension into ITF, cheek, or posterior to pterygoid plates || Erosion of skull base<br><br>'''IIIa''': Minimal skull base involvement<br>'''IIIb''': Extensive intracranial extension, with or without invasion into CS || -- || -- | | Radkowski (1996)<ref name="Radkowski 1996">Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma: changes in staging and treatment. Archives of Otolaryngology–Head & Neck Surgery. 1996 Feb 1;122(2):122-9. 10.1001/archotol.1996.01890140012004</ref>|| '''IA''': Confined to nose or NP<br>'''IB''': Extends into one or more sinuses || '''IIa''': Minimal extension into medial PMF<br>'''IIb''': Full occupation of PMF with local mass effect<br>'''IIc''': Extension into ITF, cheek, or posterior to pterygoid plates || Erosion of skull base<br><br>'''IIIa''': Minimal skull base involvement<br>'''IIIb''': Extensive intracranial extension, with or without invasion into CS || -- || -- | ||
|- | |- | ||
| Sessions (1981)<ref name="Sessions 1981">Sessions RB, Bryan RN, Naclerio RM, Alford BR. Radiographic staging of juvenile angiofibroma. Head & neck surgery. 1981 Mar;3(4):279-83.</ref> || '''IA''': Confined to nose or NP<br>'''IB''': Extends into one or more sinuses || '''IIa''': Minimal extension into PMF<br>'''IIb''': Full occupation of PMF with or without orbital erosion<br>'''IIc''': ITF with or without cheek extension || Intracranial extension || -- || -- | | Sessions (1981)<ref name="Sessions 1981">Sessions RB, Bryan RN, Naclerio RM, Alford BR. Radiographic staging of juvenile angiofibroma. Head & neck surgery. 1981 Mar;3(4):279-83. https://doi.org/10.1002/hed.2890030404</ref> || '''IA''': Confined to nose or NP<br>'''IB''': Extends into one or more sinuses || '''IIa''': Minimal extension into PMF<br>'''IIb''': Full occupation of PMF with or without orbital erosion<br>'''IIc''': ITF with or without cheek extension || Intracranial extension || -- || -- | ||
|- | |- | ||
| UPMC (2010)<ref name="Snyderman 2010">Snyderman CH, Pant H, Carrau RL, Gardner P. A new endoscopic staging system for angiofibromas. Archives of Otolaryngology–Head & Neck Surgery. 2010 Jun 21;136(6):588-94.</ref> || Nasal cavity, medial PPF || Paranasal sinuses, lateral PPF; no residual vascularity || Skull base erosion, orbit, ITF involvement; no residual vascularity || Skull base erosion, orbit, ITF involvement; residual vascularity || Intracranial extension with residual vascularity<br><br>'''M''': Medial extension<br>'''L''': Lateral extension | | UPMC (2010)<ref name="Snyderman 2010">Snyderman CH, Pant H, Carrau RL, Gardner P. A new endoscopic staging system for angiofibromas. Archives of Otolaryngology–Head & Neck Surgery. 2010 Jun 21;136(6):588-94. 10.1001/archoto.2010.83</ref> || Nasal cavity, medial PPF || Paranasal sinuses, lateral PPF; no residual vascularity || Skull base erosion, orbit, ITF involvement; no residual vascularity || Skull base erosion, orbit, ITF involvement; residual vascularity || Intracranial extension with residual vascularity<br><br>'''M''': Medial extension<br>'''L''': Lateral extension | ||
|- | |- | ||
|+ style="caption-side:bottom; font-weight: normal;"|''Abbreviations: Cavernous sinus (CS), Ethmoid sinus (ES), Infratemporal fossa (ITF), Internal carotid artery (ICA), Maxillary sinus (MS), Nasopharynx (NP), Optic chiasm (OC), Pituitary fossa (PF), Pterygomaxillary fissure (PMF), Pterygopalatine fossa (PPF), Sphenoid sinus (SS)'' | |+ style="caption-side:bottom; font-weight: normal;"|''Abbreviations: Cavernous sinus (CS), Ethmoid sinus (ES), Infratemporal fossa (ITF), Internal carotid artery (ICA), Maxillary sinus (MS), Nasopharynx (NP), Optic chiasm (OC), Pituitary fossa (PF), Pterygomaxillary fissure (PMF), Pterygopalatine fossa (PPF), Sphenoid sinus (SS)'' | ||
Revision as of 17:40, 17 November 2024
Overview
Juvenile nasopharyngeal angiofibroma (JNA) is a benign vascular neoplasm of the nasal cavity and nasopharynx that classically presents in adolescent boys.
Pathophysiology
Relevant Anatomy
JNA's typically originate in the region of the sphenopalatine artery (SPA) in the posterior nasal cavity/nasopharynx. From there, they can extend into the paranasal sinuses, pterygopalatine fossa (PPF), infratemporal fossa (ITF), orbit, or cranial vault.
-
Cadaveric model of the PPF
-
Neural contents of the PPF
-
Maxillary artery branches, with SPA at the distal end
-
Location of the sphenopalatine foramen
-
Location of the ITF
Disease Etiology
Epidemiology
Juvenile nasopharyngeal angiofibroma has been reported to be the most common benign neoplasm of the nasopharynx in young males. It accounts for 0.05% to 0.5% of all head and neck tumors, with a reported incidence of 1 in 5,000 to 1 in 60,000 in the US annually.[1][2][3] It classically presents in adolescent males, with an typical age of presentation between 13 and 22 years old.[4]
Genetics
There is no identified definitive genetic locus that predisposes patients to JNA's. However, there have been a number of studies looking at the various genetic components that could influence their formation.[5] Due to fact that JNA's classically form in adolescent males, there have been several studies focused on the possible hormonal influence on their formation and growth. JNA's tend to have an abundance of progesterone and estradiol, but a relatively lower concentration of testosterone and dihydrotestosterone.[6][7] Supplemental testosterone was trialed in JNA patients, but both tumor growth[8] and tumor recurrence[9] have been documented.
Histology
Diagnosis
Patient History
Patients may have a history of any of the following symptoms:
- Unilateral nasal obstruction
- Recurrent epistaxis
- High-volume epistaxis
- Eustachian tube dysfunction
- Headache
- Facial swelling
- Anosmia / Hyposmia
- Cranial neuropathy
- Vision changes
Physical Examination
Many patients will not have obvious findings on anterior rhinoscopy. A large vascular-appearing mass is commonly fond on nasal endoscopy on the posterior lateral nasal sidewall near the region of the sphenopalatine artery. Note that these hypervascular masses should not be biopsied, as this may result in significant bleeding that is hard to control in the clinic setting.
Laboratory Tests
Laboratory tests are not commonly useful in the diagnosis of JNA's, but should be performed preoperatively in the case of a planned surgical resection.
- Hemoglobin / Hematocrit
- Platelet level
- Platelet function (if family history of platelet dysfunction)
- PT / INR
- Blood Type and Screen (all patients)
- Blood Type and Cross (patients with advanced stage tumors where a significant blood loss is expected)
Imaging
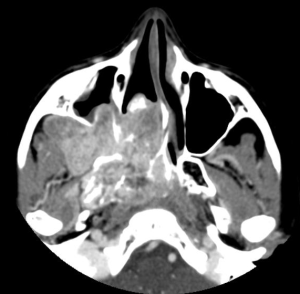
CT scan, angiography, and MRI are all useful in the workup of JNA's and have differing benefits.[10] CT is typically the first imaging modality ordered in these patients, and is helpful for delineating the extent of bony erosion. Angiography demonstrates the extent of the mass well, and is frequently used in pre-operative embolization 24-48 hours before surgical resection. A majority of JNA's are supplied by the external carotid system, either by the maxillary artery (SPA) or the ascending pharyngeal artery.[10] A lesser fraction of tumors are supplied by the internal carotid system (ophthalmic or sphenoidal branches), and this is typically in larger masses with intracranial invasion. MRI can be used to assess for intraorbital or intracranial extension. JNA's are T1 intermediate, T2 heterogenous with flow voids, and enhance with Gadolinium. The following are general characteristics often found in imaging of JNA's:
- Highly vascular nasopharyngeal mass
- Holman-Miller Sign[11]: Anterior displacement of the posterior maxillary wall due to mass effect from the tumor
- Widening of the PMF or PPF
- Erosion of the pterygoid plate, especially the medial plate
There are several classification systems that have been proposed for JNAs based on imaging findings.
| Classification System | Stage I | Stage II | Stage III | Stage IV | Stage V |
|---|---|---|---|---|---|
| Andrews (1989)[12] | Confined to NP | Invading one of the following with evidence of bony erosion: PPF, MS, ES, or SS | Invading ITF or orbit IIIa: No intracranial extension IIIb: Extradural (parasellar) extension |
Intradural extension IVa: No infiltration of CS, PF, or OC IVb: Infiltration of CS, PF, or OC |
-- |
| Chandler (1984)[13] | Confined to NP | Extension into the nasal cavity, SS, or both | Extension into any of the following: antrum, ES, PMF, ITF, orbit, or cheek | Intracranial extension | -- |
| Onerci (2006)[14] | Nose, NP, ES, and SS or minimal extension into PMF | MS involvement, full occupation of PMF, extension to anterior cranial fossa, limited extension into ITF | Deep extension into cancellous bone at pterygoid base or body and GW of sphenoid, significant lateral extension into ITF or pterygoid plates, orbital involvement, CS obliteration | Intracranial extension between pituitary gland and ICA, tumor localization lateral to ICA, middle fossa extension and extensive intracranial extension | -- |
| Radkowski (1996)[15] | IA: Confined to nose or NP IB: Extends into one or more sinuses |
IIa: Minimal extension into medial PMF IIb: Full occupation of PMF with local mass effect IIc: Extension into ITF, cheek, or posterior to pterygoid plates |
Erosion of skull base IIIa: Minimal skull base involvement IIIb: Extensive intracranial extension, with or without invasion into CS |
-- | -- |
| Sessions (1981)[16] | IA: Confined to nose or NP IB: Extends into one or more sinuses |
IIa: Minimal extension into PMF IIb: Full occupation of PMF with or without orbital erosion IIc: ITF with or without cheek extension |
Intracranial extension | -- | -- |
| UPMC (2010)[17] | Nasal cavity, medial PPF | Paranasal sinuses, lateral PPF; no residual vascularity | Skull base erosion, orbit, ITF involvement; no residual vascularity | Skull base erosion, orbit, ITF involvement; residual vascularity | Intracranial extension with residual vascularity M: Medial extension L: Lateral extension |
Differential Diagnosis
In the case of a nasopharyngeal mass, the following should also be considered:
- Clival chondroma
- Encephalocele
- Esthesioneuroblastoma
- Inverted papilloma
- Nasal polyp
- Nasopharyngeal carcinoma
- Nasopharyngeal teratoma
- Rhabdomyosarcoma
- Vascular malformation
Management
Medical Management
Surgical Management
Outcomes
Complications
Prognosis
References
- ↑ Boghani Z, Husain Q, Kanumuri VV, Khan MN, Sangvhi S, Liu JK, Eloy JA. Juvenile nasopharyngeal angiofibroma: a systematic review and comparison of endoscopic, endoscopic‐assisted, and open resection in 1047 cases. The Laryngoscope. 2013 Apr;123(4):859-69. https://doi.org/10.1002/lary.23843
- ↑ Ferouz AS, Mohr RM, Paul P. Juvenile nasopharyngeal angiofibroma and familial adenomatous polyposis: an association?. Otolaryngology—Head and Neck Surgery. 1995 Oct;113(4):435-9. https://doi.org/10.1016/S0194-59989570081-1
- ↑ Huang Y, Liu Z, Wang J, Sun X, Yang L, Wang D. Surgical management of juvenile nasopharyngeal angiofibroma: analysis of 162 cases from 1995 to 2012. The Laryngoscope. 2014 Aug;124(8):1942-6. https://doi.org/10.1002/lary.24522
- ↑ Newman M, Nguyen TB, McHugh T, Reddy K, Sommer DD. Early-onset juvenile nasopharyngeal angiofibroma (JNA): a systematic review. Journal of Otolaryngology-Head & Neck Surgery. 2023 Dec;52(1):s40463-023. https://doi.org/10.1186/s40463-023-00687-w
- ↑ Doody J, Adil EA, Trenor III CC, Cunningham MJ. The genetic and molecular determinants of juvenile nasopharyngeal angiofibroma: a systematic review. Annals of Otology, Rhinology & Laryngology. 2019 Nov;128(11):1061-72. https://doi.org/10.1177/0003489419850194
- ↑ Kumagami H. Estradiol, dihydrotestosterone, and testosterone in juvenile nasopharyngeal angiofibroma tissue. American Journal of Rhinology. 1993 May;7(3):101-4. https://doi.org/10.2500/105065893781976393
- ↑ Kumagami H. Sex hormones in juvenile nasopharyngeal angiofibroma tissue. Auris Nasus Larynx. 1993 Jan 1;20(2):131-5. https://doi.org/10.1016/S0385-8146(12)80240-9
- ↑ Johnsen S, Kloster JH, Schiff M. The action of hormones on juvenile nasopharyngeal angiofibroma. Acta Oto-Laryngologica. 1966 Jan 1;61(1-6):153-60. https://doi.org/10.3109/00016486609127052
- ↑ Riggs S, Orlandi RR. Juvenile nasopharyngeal angiofibroma recurrence associated with exogenous testosterone therapy. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck. 2010 Jun;32(6):812-5. https://doi.org/10.1002/hed.21152
- ↑ 10.0 10.1 Gaillard F, Walizai T, Bell D, et al. Juvenile nasopharyngeal angiofibroma. Reference article, Radiopaedia.org (Accessed on 17 Nov 2024) https://doi.org/10.53347/rID-1541
- ↑ Niknejad M, Tatco V, Bell D, et al. Holman-Miller sign (maxillary sinus). Reference article, Radiopaedia.org (Accessed on 17 Nov 2024) https://doi.org/10.53347/rID-21804
- ↑ Andrews JC, Fisch U, Aeppli U, Valavanis A, Makek MS. The surgical management of extensive nasopharyngeal angiofibromas with the infratemporal fossa approach. The Laryngoscope. 1989 Apr;99(4):429-37. https://doi.org/10.1288/00005537-198904000-00013
- ↑ Chandler JR, Moskowitz L, Goulding R, Quencer RM. Nasopharyngeal angiofibromas: staging and management. Annals of Otology, Rhinology & Laryngology. 1984 Jul;93(4):322-9. https://doi.org/10.1177/000348948409300408
- ↑ Onerci M, Oğretmenoğlu O, Yücel T. Juvenile nasopharyngeal angiofibroma: a revised staging system. Rhinology. 2006 Mar 1;44(1):39-45. PMID: 16550949
- ↑ Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma: changes in staging and treatment. Archives of Otolaryngology–Head & Neck Surgery. 1996 Feb 1;122(2):122-9. 10.1001/archotol.1996.01890140012004
- ↑ Sessions RB, Bryan RN, Naclerio RM, Alford BR. Radiographic staging of juvenile angiofibroma. Head & neck surgery. 1981 Mar;3(4):279-83. https://doi.org/10.1002/hed.2890030404
- ↑ Snyderman CH, Pant H, Carrau RL, Gardner P. A new endoscopic staging system for angiofibromas. Archives of Otolaryngology–Head & Neck Surgery. 2010 Jun 21;136(6):588-94. 10.1001/archoto.2010.83




